Abstract
Objective
Quantify the evolution and severity of neonatal skin injury, specifically diaper skin compromise, by embedding a validated skin integrity evaluation into the electronic health record (EHR).
Methods
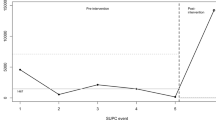
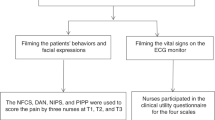
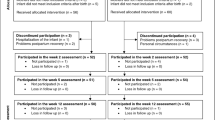
Retrospective longitudinal cohort analysis of 747 patients stratified by gestation: 22–27, 28–31, 32–24, and 35–37 weeks, from birth to discharge. Primary outcomes were time to first perineal erythema, duration as percent days with erythema, and severity as maximum score. Data were analyzed using generalized linear models and multiple linear regression methods.
Results
Seventy percent had erythema and, of these, 34% had at least one high score with bleeding. Days with erythema ranged from 34–44% (p < 0.05). Days to first erythema were inversely correlated with gestational age. Risks for severe injury included short time to first erythema, 5 or more stools/day, infection, and Caucasian race/ethnicity.
Conclusions
The EHR-based scale can be readily implemented to mitigate diaper skin compromise in premature infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated from the EHR and data analysis are not available publicly due to patient privacy restrictions and regulations. A limited, de-identified dataset may be available from the corresponding author upon reasonable request.
References
Visscher MO, Narendran V, Pickens WL, LaRuffa AA, Meinzen-Derr J, Allen K, et al. Vernix caseosa in neonatal adaptation. J Perinatol. 2005;25:440–6.
Cartlidge P. The epidermal barrier. Semin Neonatol. 2000;5:273–80.
Evans NJ, Rutter N. Development of the epidermis in the newborn. Biol Neonate. 1986;49:74–80.
Rutter N. Clinical consequences of an immature barrier. Semin Neonatol. 2000;5:281–7.
Malik A, Witsberger E, Cottrell L, Kiefer A, Yossuck P. Perianal dermatitis, its incidence, and patterns of topical therapies in a level IV neonatal intensive care unit. Am J Perinatol. 2018;35:486–93.
Visscher M, Odio M, Taylor T, White T, Sargent S, Sluder L, et al. Skin care in the NICU patient: effects of wipes versus cloth and water on stratum corneum integrity. Neonatology. 2009;96:226–34.
Al-Waili NS. Clinical and mycological benefits of topical application of honey, olive oil and beeswax in diaper dermatitis. Clin Microbiol Infect. 2005;11:160–3.
Berg RW. Etiologic factors in diaper dermatitis: a model for development of improved diapers. Pediatrician. 1987;14 Suppl 1:27–33.
Berg RW. Etiology and pathophysiology of diaper dermatitis. Adv Dermatol. 1988;3:75–98.
Berg RW, Buckingham KW, Stewart RL. Etiologic factors in diaper dermatitis: the role of urine. Pediatr Dermatol. 1986;3:102–6.
Berg RW, Milligan MC, Sarbaugh FC. Association of skin wetness and pH with diaper dermatitis. Pediatr Dermatol. 1994;11:18–20.
Davis JA, Leyden JJ, Grove GL, Raynor WJ. Comparison of disposable diapers with fluff absorbent and fluff plus absorbent polymers: effects on skin hydration, skin pH, and diaper dermatitis. Pediatr Dermatol. 1989;6:102–8.
Honig PJ, Gribetz B, Leyden JJ, McGinley KJ, Burke LA. Amoxicillin and diaper dermatitis. J Am Acad Dermatol. 1988;19:275–9.
Atherton DJ. The aetiology and management of irritant diaper dermatitis. J Eur Acad Dermatol Venereol. 2001;15 Suppl 1:1–4.
Mugita Y, Minematsu T, Huang L, Nakagami G, Kishi C, Ichikawa Y, et al. Histopathology of incontinence-associated skin lesions: inner tissue damage due to invasion of proteolytic enzymes and bacteria in macerated rat skin. PLoS ONE. 2015;10:e0138117.
Beverly RL, Huston RK, Markell AM, McCulley EA, Martin RL, Dallas DC. Milk peptides survive in vivo gastrointestinal digestion and are excreted in the stool of infants. J Nutr. 2020;150:712–21.
Munch A, Garten L, Buhrer C. Protracted maturation of pancreatic-specific elastase 1 excretion in preterm infants of extremely low gestational age. J Pediatr Gastroenterol Nutr. 2013;56:532–6.
Dunk AM, Broom M, Fourie A, Beeckman D. Clinical signs and symptoms of diaper dermatitis in newborns, infants, and young children: a scoping review. J Tissue Viability. 2022;31:404–15.
Esser MS, Ngui EM, Johnson TS. Contributing factors to diaper dermatitis and NICU length of stay. J Neonatal Nurs. 2021;27:358–64.
Hess CT. Electronic health record wound care checklists. Adv Skin Wound Care. 2012;25:288.
Monfre J, Batchelor F, Skar A. Improving skin assessment documentation in the electronic health record to prevent perioperative pressure injuries. AORN J. 2022;115:53–63.
Montague M, Karafa M, Albert NM. Assessment and documentation of incontinence-associated dermatitis after implementation of a standardised instrument: a comparative study. J Wound Care. 2019;28:S4–11.
Elsner P. Skin Color. In: Berardesca E, Elsner, P, Wilhelm, KP, Maibach, HI, editors. Bioengineering of the skin: methods and instrumentation. Boca Raton, FL: CRC Press; 1995. p. 29–40.
Visscher M. A practical method for rapid measurement of skin condition. Newborn Infant Nurs Rev. 2014;14:147–52.
Jordan WE, Lawson KD, Berg RW, Franxman JJ, Marrer AM. Diaper dermatitis: frequency and severity among a general infant population. Pediatr Dermatol. 1986;3:198–207.
Odio MR, O'Connor RJ, Sarbaugh F, Baldwin S. Continuous topical administration of a petrolatum formulation by a novel disposable diaper. 2. Effect on skin condition. Dermatology. 2000;200:238–43.
Agren J, Sjors G, Sedin G. Transepidermal water loss in infants born at 24 and 25 weeks of gestation. Acta Paediatr. 1998;87:1185–90.
Sedin G, Hammarlund K, Stromberg B. Transepidermal water loss in full-term and pre-term infants. Acta Paediatr Scand Suppl. 1983;305:27–31.
Kalia YN, Nonato LB, Lund CH, Guy RH. Development of skin barrier function in premature infants. J Invest Dermatol. 1998;111:320–6.
Lundov MD, Krongaard T, Menne TL, Johansen JD. Methylisothiazolinone contact allergy: a review. Br J Dermatol. 2011;165:1178–82.
Dutta S, Singh B, Chessell L, Wilson J, Janes M, McDonald K, et al. Guidelines for feeding very low birth weight infants. Nutrients. 2015;7:423–42.
Csoma ZR, Meszes A, Abraham R, Kemeny L, Talosi G, Doro P. Iatrogenic skin disorders and related factors in newborn infants. Pediatr Dermatol. 2016;33:543–8.
Migoto MT, de Souza S, Rossetto EG. Skinn lesions of newborns in a neonatal unit: Descriptive study. Online Braz J Nurs. 2013;12:377–92.
Jani P, Mishra U, Buchmayer J, Maheshwari R, D'Cruz D, Walker K, et al. Global variation in skin injures and skincare practices in extremely preterm infants. World J Pediatr. 2023;19:139–57.
Lowe JR, Raugi GJ, Reiber GE, Whitney JD. Does incorporation of a clinical support template in the electronic medical record improve capture of wound care data in a cohort of veterans with diabetic foot ulcers? J Wound Ostomy Cont Nurs. 2013;40:157–62.
Khalil H, Cullen M, Chambers H, Carroll M, Walker J. Reduction in wound healing times, cost of consumables and number of visits treated through the implementation of an electronic wound care system in rural Australia. Int Wound J. 2016;13:945–50.
Visscher MO, Taylor T, Narendran V. Neonatal intensive care practices and the influence on skin condition. J Eur Acad Dermatol Venereol. 2013;27:486–93.
Burdall O, Willgress L, Goad N. Neonatal skin care: developments in care to maintain neonatal barrier function and prevention of diaper dermatitis. Pediatr Dermatol. 2019;36:31–5.
Pratt AG. Perianal dermatitis of the newborn. AMA Am J Dis Child. 1951;82:429–32.
Carr AN, DeWitt T, Cork MJ, Eichenfield LF, Folster-Holst R, Hohl D, et al. Diaper dermatitis prevalence and severity: global perspective on the impact of caregiver behavior. Pediatr Dermatol. 2020;37:130–6.
Man MQ, Lin TK, Santiago JL, Celli A, Zhong L, Huang ZM, et al. Basis for enhanced barrier function of pigmented skin. J Invest Dermatol. 2014;134:2399–407.
Visscher MO, Summers A, Narendran V, Khatry S, Sherchand J, LeClerq S, et al. Birthweight and environmental conditions impact skin barrier adaptation in neonates receiving natural oil massage. Biomed Hub. 2021;6:17–24.
Carr LH, Christ L, Ferro DF. The electronic health record as a quality improvement tool: exceptional potential with special considerations. Clin Perinatol. 2023;50:473–88.
Visscher MO, McKeown K, Nurre M, Strange R, Mahan T, Kinnett M, et al. Skin care for the extremely low-birthweight infant. Neoreviews. 2023;24:e229–42.
Acknowledgements
The authors wish to thank the members of the electronic medical record clinical team, Kelly Mathis, for her work on the skin evaluation algorithm and to the clinical staff for their technical support.
Author information
Authors and Affiliations
Contributions
The author contributions are as follows. MV and VN conceptualized the project and study design. MV, VN, AT, MN, RS, MK, and KM contributed to the data acquisition, data interpretation, critical review of the manuscript, and final approval of the version being submitted. MV and KM conducted the data analysis. MV, VN, and AT drafted and revised the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Visscher, M.O., Taleghani, A., Nurre, M. et al. Assessment of diaper dermatitis using a novel electronic health record-embedded scale. J Perinatol 44, 501–507 (2024). https://doi.org/10.1038/s41372-023-01824-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01824-z